TEACHING CIRCULATORY
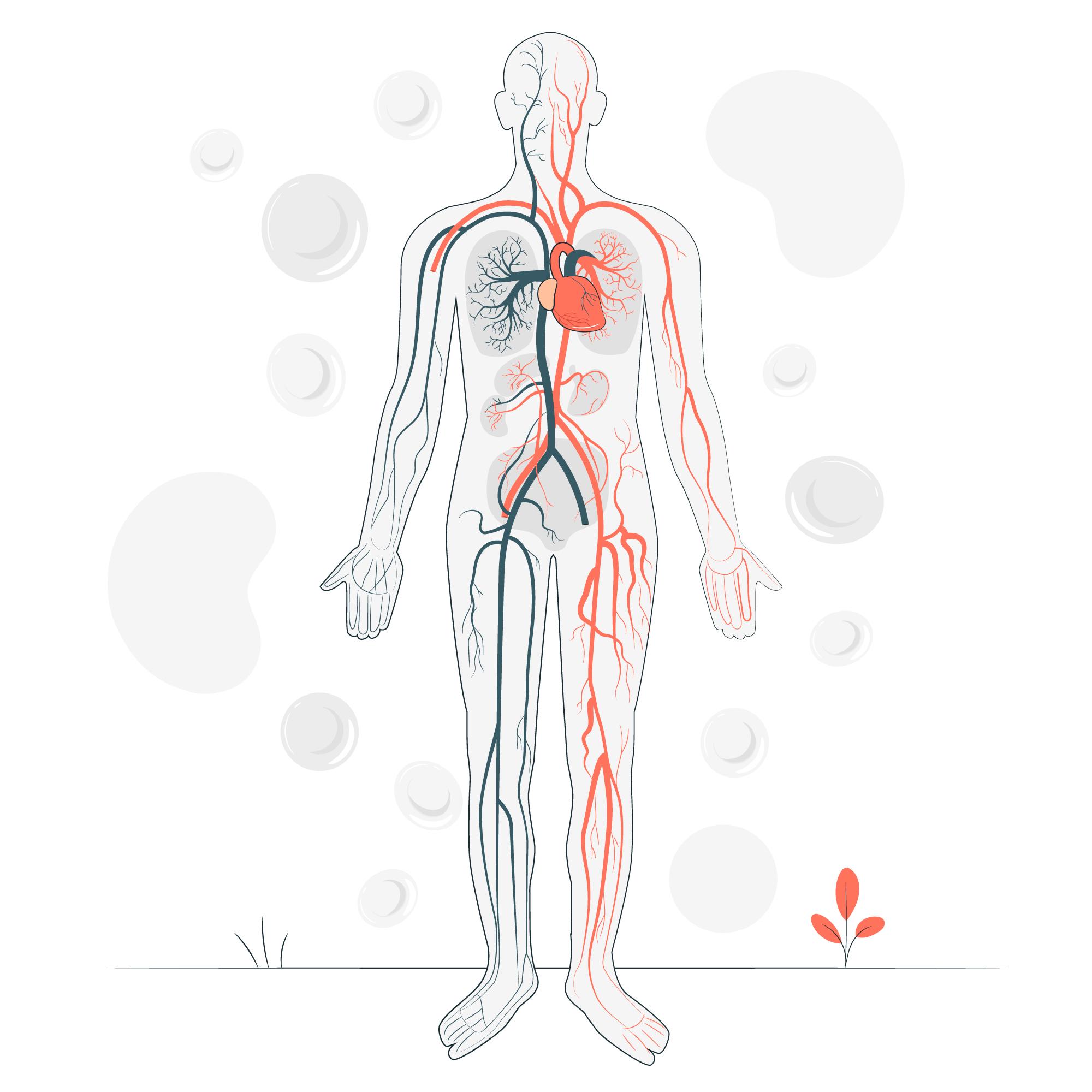
HTN
Blood Pressure Levels
SN instructed patient/caregiver about High blood pressure. Normal blood pressure is when your blood pressure is lower than 120/80 mmHg most of the time. High blood pressure (hypertension) is when your blood pressure is 140/90 mmHg or above most of the time. Both numbers in a blood pressure reading are important. But after age 50, the systolic reading is even more important. Isolated systolic hypertension is a condition in which the diastolic pressure is normal (less than 80 mm Hg) but systolic pressure is high (greater than or equal to 130 mm Hg). This is a common type of high blood pressure among people older than 65.
HTN Signs and Symptoms
SN instructed patient/caregiver about to recognize signs and symptoms of high blood pressure, although it is frequently asymptomatic, symptoms like blurring of vision, fatigue, nose bleeds and chest pain. If symptoms continue go to ER, or call 911.
Hypertensive Heart Disease
SN educated Pt/CG that Hypertensive heart disease refers to heart conditions caused by high blood pressure. The heart working under increased pressure causes some different heart disorders. Hypertensive heart disease can lead to complications such as: thickening of the heart muscle, coronary artery disease, chronic kidney disease and other conditions such as heart failure if not controlled. Follow your MD’s orders for Heart Healthy diet, exercise as tolerated and take medications as prescribed.
HTN managing/controlling I
SN instructed patient/caregiver on some measures aimed to managing/controlling hypertension, such as: monitoring blood pressure regularly, eating low sodium diet, increase more fruits to increase your potassium, walk daily for 30 minutes, and have regular check-ups and take medications exactly as directed by MD.
HTN managing/controlling II
SN instructed patient/caregiver how can do many things to help control the blood pressure at home, including: Eat a heart-healthy diet, including potassium and fiber, and drink plenty of water, exercise regularly at least 30 minutes of aerobic exercise a day, limit the amount of sodium (salt) you eat and aim for less than 1,500 mg per day and reduce stress.
HTN Risk Factors
SN educated Pt/ CG on hypertension; high blood pressure has many risk factors, including: Age, Race, Family history, being overweight or obese, not being physically active, using tobacco, too much salt (sodium) in your diet, too little potassium in your diet, drinking too much alcohol, Stress and certain chronic conditions (kidney disease, diabetes and sleep apnea).
HTN Complications
SN educated Pt/ CG on hypertension; the excessive pressure on your artery walls caused by high blood pressure can damage your blood vessels as well as your organs. The higher your blood pressure and the longer it goes uncontrolled, the greater the damage. Uncontrolled high blood pressure can lead to complications including: Heart attack or stroke, Aneurysm, Heart failure, Weakened and narrowed blood vessels in your kidneys, Thickened, narrowed or torn blood vessels in the eyes, Metabolic syndrome, Trouble with memory or understanding and Dementia.
High Blood Pressure (hypertension)
SN educated Pt/CG that High blood pressure (hypertension) is a common condition in which the long-term force of the blood against your artery walls is high enough that it may eventually cause health problems, such as heart disease. Blood pressure is determined both by the amount of blood your heart pumps and the amount of resistance to blood flow in your arteries. Generally, the hypertension is treated with exercises, salt restriction and medication.
Hypertensive Urgency
SN instructed patient and caregiver on hypertensive urgency which is a situation where the blood pressure is severely elevated or higher for your diastolic pressure and that experiencing hypertensive urgency may or may not experience one or more of these symptoms: severe headache, shortness of breath, nosebleeds, and severe anxiety, chest or back pain, numbness or severe weakness, change in vision or difficulty speaking. Patient and caregiver were advised to seek immediately medical assistance and/or call 9-1-1 if any of these signs or symptoms appear.
Home Monitoring Equipment
SN instructed patient/caregiver about what way and at what time to take blood pressure measurements using home monitoring equipment. The patient was instructed to take blood pressure at the same time each day, have a record of blood pressure readings. Devices that measure your blood pressure at your wrist or finger aren’t recommended by the American Heart Association because they can provide less reliable results.
CHF
Congestive Heart Failure I
SN educated patient/caregiver that heart failure, also called Congestive Heart Failure (CHF), means your heart does not pump blood as well as it should. This does not mean your heart has stopped working, but that it is not as strong as it used to be and fluid builds up in the lungs and other parts of your body. This can cause shortness of breath, swelling in the legs, feet, and stomach. Heart failure starts slowly and can get worse over time.
Congestive Heart Failure II
SN educated patient/caregiver about the heart is a muscle that pumps oxygen-rich blood to all parts of the body. When you have heart failure, the heart is not able to pump as well as it should. Blood and fluid may back up into the lungs (congestive heart failure), and some parts of the body don’t get enough oxygen-rich blood to work normally. These problems lead to the symptoms of heart failure. Follow a heart healthy diet. And make sure to limit the salt (sodium) in your diet. Salt causes your body to hold water. This makes your heart work harder as there is more fluid for the heart to pump. This makes that fluid builds up in the lungs and other parts of your body. This can cause shortness of breath, swelling in the legs, feet, and stomach. Heart failure starts slowly and can get worse over time.
CHF Symptoms and Signs
SN explained patient/caregiver that the symptoms and signs of congestive heart failure (CHF) may include: Shortness of breath (also called dyspnea) most commonly during activity, at rest, or while sleeping, which may come on suddenly and wake you up. You often have difficulty breathing while lying flat and may need to prop up the upper body and head on two pillows. You often complain of waking up tired or feeling anxious and restless. Blood backs up in the pulmonary veins (the vessels that return blood from the lungs to the heart) because the heart can’t keep up with the supply. This causes fluid to leak into the lungs. Persistent coughing or wheezing, coughing that produces white or pink blood – tinged mucus. Fluid builds up in the lungs. Buildup of excess fluid in body tissues (edema) swelling in the feet, ankles, legs or abdomen or weight gain. You may find that your shoes feel tight.
CHF Medical Emergency
SN instructed patient/caregiver about the signs and symptoms to call 9-1-1 with regard to diagnosis Congestive Heart Failure (CHF), that may point to the condition being worsened and needing immediate medical attention: crackling noise that can be audibly heard as patient exhales, pink, frothy sputum that patient coughs out, patient has markedly increased shortness of breath that is not relieved even after 15 minutes of rest, may also be non-productive but incessant cough that includes crackling sound, rapid heart rate that may last more than 30 minutes (with or without dizziness), weight gain of more than 2-3 pounds in one day, or 5-7 pounds in seven days, lower extremity swelling which may or may not include fluid seeping through the skin. With regard to increased/increasing shortness of breath that is not relieved, however, told to patient and caregiver to remain calm and call 9-1-1 and not wait as it needs to be taken care of right away, because the patient needs oxygen in the body immediately (a medical emergency).
CHF Complications
SN instructed patient/caregiver about on some potential complications of Congestive Heart Failure (CHF), such as: acute pulmonary edema and pneumonia, kidney damage or failure, heart valve problems, heart rhythm problems, liver damage. Complications of heart failure depend on the severity of heart disease, your overall health and other factors such as your age.
CHF Prevention
SN instructed patient/caregiver about prevention of CHF. The key to preventing heart failure is to reduce your risk factors. You can control or eliminate many of the risk factors for heart disease by making healthy lifestyle changes and by taking the medications prescribed by your doctor. Lifestyle changes you can make to help prevent heart failure include: not smoking, controlling certain conditions, such as high blood pressure and diabetes, staying physically active, eating healthy foods, maintaining a healthy weight, reducing and managing stress.
ANGINA
Angina Pectoris I
SN educated patient and caregiver about what angina pectoris is. Angina pectoris is chest pain that is caused by insufficient oxygen to meet demands of the heart. Lack of oxygen occurs when insufficient blood flows through the coronary arteries. Stable angina usually has a precipitating cause while unstable angina can occur at rest.
Angina Symptoms
SN instructed patient and caregiver about angina symptoms include chest pain and discomfort, possibly described as pressure, squeezing, burning or fullness. You may also have pain in your arms, neck, jaw, shoulder or back. Other symptoms that you may have with angina include: dizziness, fatigue, nausea, shortness of breath, sweating. These symptoms need to be evaluated immediately by a doctor who can determine whether you have stable angina, or unstable angina, which can be a precursor to a heart attack.
Stable Angina
SN instructed patient and caregiver about characteristics of stable angina. Develops when your heart works harder, such as when you exercise or climb stairs. Can usually be predicted and the pain is usually similar to previous types of chest pain you’ve had. Lasts a short time, perhaps five minutes or less. Disappears sooner if you rest or use your angina medication. Stable angina is the most common form of angina.
Unstable Angina
SN instructed patient and caregiver about characteristics of unstable angina (a medical emergency). Occurs even at rest. Is a change in your usual pattern of angina? Is unexpected. Is usually more severe and lasts longer than stable angina, maybe 30 minutes or longer. May not disappear with rest or use of angina medication. Might signal a heart attack. Call 911 or emergency medical help.
Angina Risk Factors
SN instructed patient and caregiver about risk factors increase your risk of coronary artery disease and angina: high blood pressure, high blood cholesterol or triglyceride levels, tobacco, diabetes, family history of heart disease, older age, lack of exercise, stress, obesity.
Angina Prevention
SN instructed patient and caregiver about the prevention of angina by making the same lifestyle changes that might improve your symptoms. These include: quitting smoking, monitoring and controlling other health conditions (high blood pressure, high cholesterol and diabetes), eating a healthy diet and maintaining a healthy weight, increasing your physical activity after you get your doctor’s OK, reducing stress level, limiting alcohol consumption, getting an annual flu shot to avoid heart complications from the virus.
DEVICES
Sleeping with LVAD (Left Ventricular Assist Devices)
SN taught patient/caregiver on sleeping with LVAD, and it was explained that many LVAD patients actually find that they’re able to sleep more comfortably with their LVAD than they did before because they’re feeling better and breathing more easily. There are, however, two major ways that having an LVAD affects your sleep routine: You may not be able to sleep on your stomach. Stomach sleeping can compress or pull on the driveline. Sleeping on your back is the best option, although some LVAD patients find it comfortable to sleep on their sides. You’ll also need to make sure that the driveline doesn’t get tangled in clothing or blankets. At first, sleeping with the LVAD may feel awkward, but most patients get used to it after a few days.
Experience with LVAD
SN instructed patient/caregiver that it is not uncommon to experience significant stress, anxiety or depression when receiving your LVAD or becoming a caregiver for an LVAD recipient. There have been a lot of changes in your body and your life recently. There are many different causes of mental health issues, many of which are not under your control. If you are experiencing symptoms of depression or anxiety, it is not a bad thing to ask for help. There are many new medications and treatments available to help you feel better. Sometimes mental health issues are not recognized by the person who is affected. We have provided this tool to help or a loved one identify when you may need to ask for help.
LVAD Nutritional Guidelines
SN instructed patient/caregiver that certain medications you might be taking, including Coumadin (Warfarin Sodium Tablets); also require special nutritional precautions. Your doctor or LVAD coordinator can provide you with detailed nutritional guidelines for your particular situation.
LVAD healthy living
SN instructed patient/caregiver that for healthy living with your LVAD, you’ll need to make sure that: the equipment is working properly, you have sufficient power sources at all times, your driveline exit site is clean and dry, following a healthy diet, exercising regularly, as you’re able to tolerate it, are taking your medications and supplements as directed by your doctor.
LVAD Instructions
SN instructed patient/caregiver about his/her LVAD team will give you detailed instructions on what you need to do on a daily basis for your specific device and medical condition. They will also most likely give you a chart (sometimes called a “flowsheet”) customized for your specific device, to fill out daily. Flowsheets make it easy to keep track of your weight, medications, device settings (such as pump speed, power, etc.) and other daily maintenance items. Sample flowsheets are included at the bottom of the page (they vary slightly based on manufacturer). It is a sample only; use the flowsheet provided by your LVAD team.
Traveling with an LVAD
SN instructed patient/caregiver that when traveling with an LVAD will involve some extra planning and preparation when scheduling a trip, discuss your plans ahead of time with your LVAD team. They ‘ll help you be as independent as possible, and still stay safe and healthy. They can also provide you with the necessary travel documents, as well as helpful tips and medical condition. They will also most likely give you a chart (sometimes called a “flowsheet”) customized for your specific device, to fill out daily. Flowsheets make it easy to keep track of your weight, medications, device settings (such as pump speed, power, etc.) and other daily maintenance items. Sample flowsheets are included at the bottom of the page (they vary slightly based on manufacturer). It is a sample only; use the flowsheet provided by your LVAD team.
What not do with LVAD
SN instructed patient/caregiver what not do with her LVAD. Kink, bend or pull your driveline, disconnect the driveline from the controller (under normal circumstances), sleep on your stomach, take a bath or swim, play contact sports, have an MRI (CT Scans or X-Rays are OK), attempt to repair LVAD equipment yourself, leave the house without backup equipment.
Pacemaker I
SN educated patient/caregiver about pacemaker. A pacemaker is a small device that’s placed (implanted) in your chest to help control your heartbeat. It’s used to prevent your heart from beating too slowly. Implanting a pacemaker in your chest requires a surgical procedure.
Pacemaker ID
SN instructed patient/caregiver to carry your ID Card for your pacemaker with you at all times. This card will be given to you in the hospital or mailed to you. Medic Alert Bracelets are available from your pharmacist to wear at all times.
Pacemaker Postoperative
SN Instructed patient/caregiver to leave steri-strips over your site until they start to fall off. You do not need a dressing over site unless draining. Keep your incision clean and pat dry. Do not scrub. You may shower or bathe as long as your incision isn’t submerged or directly sprayed upon until well healed. For comfort, wear loose fitting clothing.
Pacemaker Follow-up
Instructed patient/caregiver to Follow-up appointments with your doctor will be discussed with you before discharge. A slight bulge will be felt at the pacemaker site. Notify your doctor if you have a fever, pain, swelling, redness, oozing, or heat at site especially if these symptoms increase after the first 3 to 4 days. Also, notify your doctor if you notice any of the following around your pacemaker site: a bruise that does not go away, soreness or yellow, green, or brown drainage from the site and any swelling from the site.
Pacemaker Instructions
SN instructed patient/caregiver to avoid activity that involves rough contact with the pacemaker site. Usual arm movement is allowed but avoid lifting your arm over your head on the pacemaker side or lifting over 10 pounds for 4 weeks. Also on the importance to take your prescribed medications as instructed. Avoid aspirin products for 2 weeks unless told otherwise.
MI
Myocardial Infarction I
SN educated patient and caregiver about a myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to a part of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Can be fatal, but treatment has improved dramatically over the years. It’s crucial to call 911 or emergency medical help.
MI Signs and Symptoms
SN instructed patient and caregiver about signs and symptoms include: pressure, tightness, pain, or a squeezing or aching sensation in your chest or arms that may spread to your neck, jaw or back, nausea, indigestion, heartburn or abdominal pain, shortness of breath, cold sweat, fatigue, lightheadedness or sudden dizziness. Not all people who have heart attacks have the same symptoms or have the same severity of symptoms.
MI Emergency Steps
SN instructed patient and caregiver about emergency medical (steps). Call for emergency medical help if you suspect you’re having a heart attack, don’t hesitate. Immediately call 911 or your local emergency number. If you don’t have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only if there are no other options. Because your condition can worsen, driving yourself puts you and others at risk. Take nitroglycerin, if prescribed to you by a doctor. Take it as instructed while awaiting emergency help. Take aspirin, if recommended. Taking aspirin during a heart attack could reduce heart damage by helping to keep your blood from clotting.
MI Ricks Factors
SN instructed patient and caregiver about factors contribute to the unwanted buildup of fatty deposits (atherosclerosis) that narrows arteries throughout your body and lead to a heart attack: high blood pressure, high blood cholesterol or triglyceride levels, tobacco, diabetes, family history of heart disease, age (men age 45 or older and women age 55 or older), lack of exercise, stress, obesity, an autoimmune condition, metabolic syndrome, illicit drug use, preeclampsia.
MI Complications
SN educated patient and caregiver about the complications are often related to the damage done to your heart during a heart attack. The most commons are: abnormal heart rhythms (arrhythmias), heart failure and sudden cardiac arrest.
MI Preventions
SN educated patient and caregiver the importance take medications can reduce your risk of a subsequent heart attack and how often you need to be monitored as medical orders. Maintain a healthy weight with a heart-healthy diet, don’t smoke, exercise regularly, manage stress and control conditions that can lead to a heart attack, such as high blood pressure, high cholesterol and diabetes are ways to prevent a heart attack.
ARRITHMIAS
Arrhythmias I
SN educated patient/caregiver about heart rhythm problems (heart arrhythmias) occur when the electrical impulses that coordinate your heartbeats don’t work properly, causing your heart to beat too fast, too slow or irregularly. Heart arrhythmias may feel like a fluttering or racing heart and may be harmless. However, some heart arrhythmias may cause bothersome — sometimes even life-threatening — signs and symptoms.
Arrhythmias Signs and Symptoms
SN educated patient/caregiver about signs and symptoms. Arrhythmias may not cause any signs or symptoms. In fact, your doctor might find you have an arrhythmia before you do, during a routine examination. Noticeable arrhythmia symptoms may include: a fluttering in your chest, a racing heartbeat (tachycardia), a slow heartbeat (bradycardia), chest pain, shortness of breath, anxiety, fatigue, lightheadedness or dizziness, sweating, fainting (syncope) or near fainting.
Arrhythmias Ricks Factors
SN instructed patient/caregiver about certain conditions may increase your risk of developing an arrhythmia as: high blood pressure, thyroid problems, coronary artery disease, other heart problems and previous heart surgery, diabetes, congenital heart disease, electrolyte imbalance, obstructive sleep apnea, alcohol, caffeine, nicotine or illegal drug use.
Arrhythmias Complications
SN instructed patient/caregiver about complications. Heart arrhythmias are associated with an increased risk of blood clots. If a clot breaks loose, it can travel from your heart to your brain. There it might block blood flow, causing a stroke. Heart failure can result if your heart is pumping ineffectively for a prolonged period due to a bradycardia or tachycardia, such as atrial fibrillation. Sometimes controlling the rate of an arrhythmia that’s causing heart failure can improve your heart’s function.
Arrhythmias Preventions
SN educated patient/caregiver about how to prevent heart arrhythmia. A heart-healthy lifestyle may include: staying physically active and keeping a healthy weight, avoiding smoking, heart-healthy diet, reducing stress, limiting or avoiding caffeine and alcohol or medications contain stimulants.
Arrhythmias Emergency
SN instructed patient/caregiver about how recognize an emergency. Some signs and symptoms may be related to your heart not pumping effectively due to the fast or slow heartbeat. These include shortness of breath, weakness, dizziness, lightheadedness, fainting or near fainting, and chest pain or discomfort. You need seek urgent medical care if you suddenly or frequently experience any of these signs and symptoms at a time when you wouldn’t expect to feel them.
CHEST PAIN
Assessment of Chest Pain
SN instructed patient/caregiver about the assessment of chest pain, including amount, frequency, location, duration and any associated symptoms. If you have new or unexplained chest pain or suspect you’re having a heart attack, call for emergency medical help immediately.
Chest Pain Presentation
SN instructed patient/caregiver about chest pain. This pain appears in many forms (from a sharp stab to a dull ache or feels crushing or burning or travels up the neck, into the jaw, and then radiates to the back or down one or both arms), and many different problems can cause chest pain. The most life-threatening causes involve the heart or lungs. Because chest pain can indicate a serious problem, it’s important to seek immediate medical help.
MISCELLANEOUS
Orthostatic hypotension
SN educated Pt/CG to Orthostatic hypotension, also known as postural hypotension: is brought on by a sudden change in body position, most often when standing, stretching or shifting from lying down to standing. This means the heart, brain, and other parts of the body do not get enough blood. This type of hypotension usually lasts only a few seconds or minutes. If you experience these symptoms, please report them to your Nurse and MD.
Heart healthy diet and lifestyle I
SN instructed patient/caregiver about a heart-healthy diet. Eating a healthy diet can reduce your risk of heart disease. A diet rich in fruits, vegetables and whole grains can help protect your heart. Beans, other low-fat sources of protein and certain types of fish. Also can reduce your risk of heart disease. Stop your activity if you feel short of breath, dizzy, or have any pain in your chest. Do not do any activity or exercise that causes pulling or pain across your chest.
Heart healthy diet and lifestyle II
SN instructed patient/caregiver about what lifestyle choices can help me feel my best: Stay active. If you are not active, your symptoms are likely to worsen quickly. Walking, and other types of physical activity help maintain your strength and improve your mood. Physical activity also helps you manage your weight. Eat heart-healthy foods and limit sodium (salt). An easy way to do this is to eat more fresh fruits and vegetables and fewer canned and processed foods.
Heart healthy Diet
SN instructed patient/caregiver about cardiac diet, as the name suggests, is often prescribed for patients who have a history of heart related problems/diseases. The cardiac diet is a healthy eating plan prepared to counter diseases such as high blood pressure, obesity, heart attack and so on. Even if a person does not suffer from a heart condition it is advisable to follow this diet as a preventive measure. Some Basic Facts about the Cardiac Diet The following are some basic facts that determine the cardiac diet. Consumption of Foods that Contain Healthy Fats Healthy Fats. Two types of fat that can be beneficial for the body are polyunsaturated fats and monounsaturated fats. Polyunsaturated fats are found in foods such as: leafy green vegetables nuts seeds fish Monounsaturated fats are said to decrease the levels of LDL or ‘bad’ cholesterol in the body. They are found in foods such as: Milk products avocado olives nuts Unhealthy Fats: One should avoid the consumption of trans fat and saturated fats. Trans fat increase the level of bad cholesterol in the body. They are often found in: packaged food items that are fried in some of the foods sold in fast food restaurants Although they help to increase the shelf life of a product they are very harmful for the body. Saturated fats are found in foods such as: cream cheese butter ghee coconut oil.

